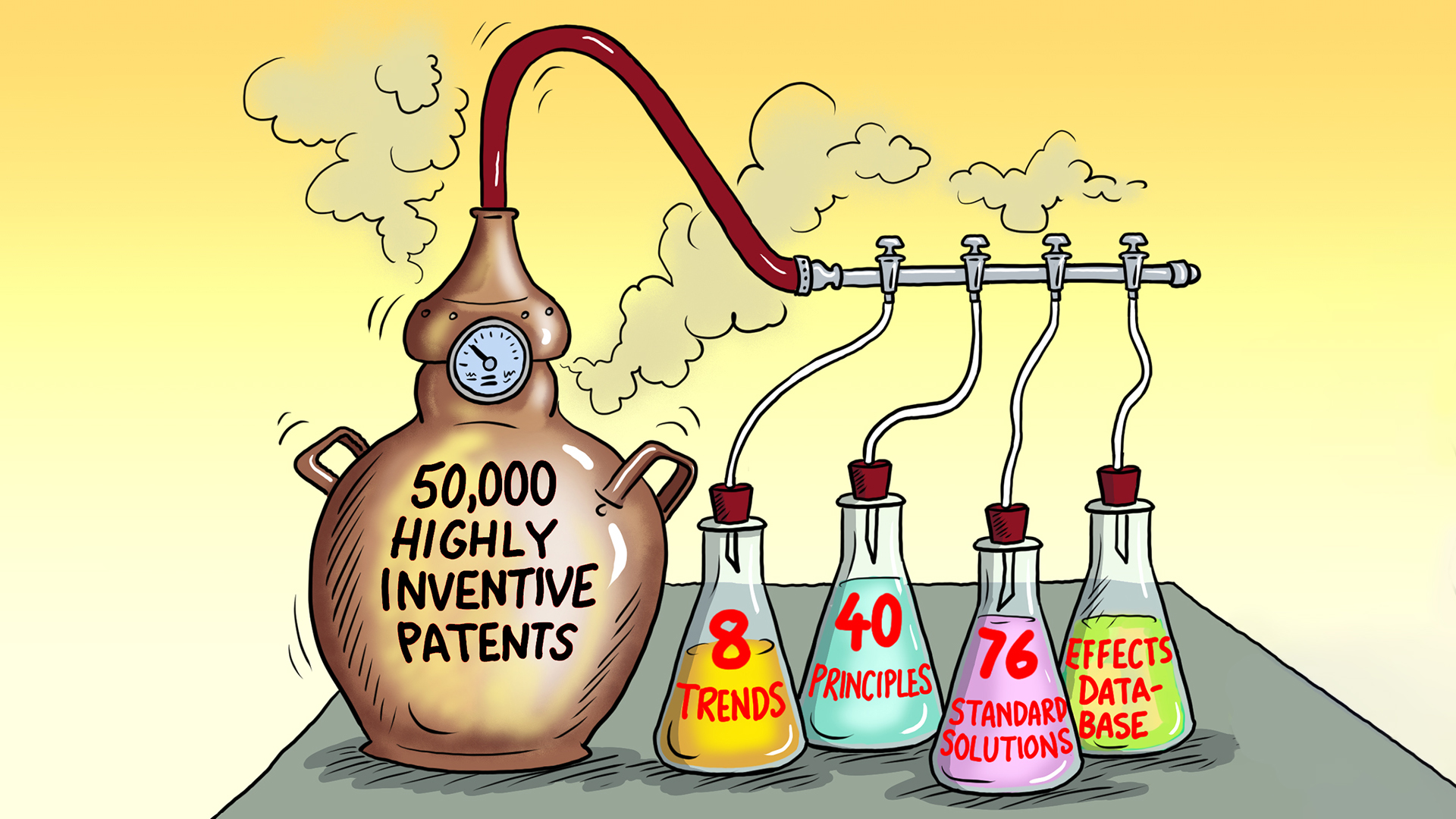
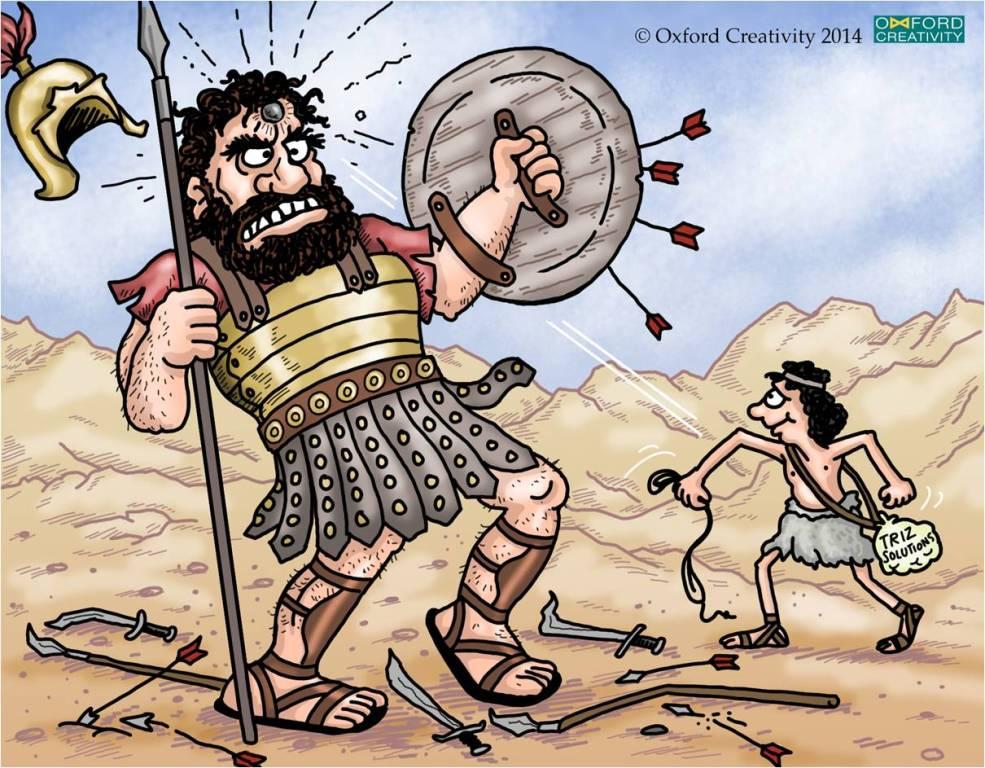
If only TRIZ was as universal as brainstorming perhaps then many more difficult problems might get resolved faster. Brainstorming is great, BUT is often quite hit and miss, which means it only works well about half the time, especially when there are challenges which are too tough or complex to be solved by brainstorming alone.
Read More